The University of Nottingham (England) has secured £801,874 in funding from the Medical Research Council (Swindon and London, England) to accelerate development of an optical fiber sensor-equipped endotracheal tube (ETT). These tubes are placed in the trachea (windpipe) in patients who need artificial breathing support. The ETT, called iTraXS, aims to prevent pressure injury to the airway and to assist with monitoring vital signs.
ETTs have an inflatable, balloon-like "cuff" that sits inside the trachea, forming a gas-tight seal to prevent leaks of oxygen-rich air and maintain effective ventilation. The seal also protects the lungs from contamination by vomit or blood, which can lead to ventilator-associated pneumonia (VAP).
Incorrect cuff inflation pressure causes two main problems. If pressure is too low, it can risk fluid getting past the cuff and causing VAP. Conversely, if pressure is too high, it can cause pressure injury in the trachea. Pressure injuries range from moderate to severe sore throat, voice change, or cough in half of all patients after surgery (0.5 million a year in the UK), to permanent scarring and narrowing of the windpipe tissue (post intubation tracheal stenosis [PITS]), which occurs in around 2000 patients annually. PITS is a disabling condition, with patients living “from breath to breath” and reporting long-term adverse impact on quality of life and multiple medical interventions.
At present, there is no medical device on the market to accurately and safely measure and monitor the contact pressure of the inflated cuff and the blood flow in the tracheal lining (mucosa). Current best practice recommends maintaining a fixed pressure in all patients. However, iTraXS enables personalized care by allowing clinical staff to find the correct pressure for each patient, balancing a good seal vs. tissue pressure and blood flow.
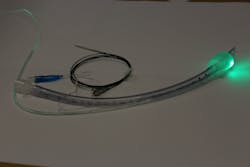
iTraXS uses thin, flexible, optical fiber sensors incorporated into a standard disposable ETT, which is linked to an optoelectronic monitoring and display unit. The device monitors both the contact pressure and the blood supply at the cuff-trachea interface (the point where the cuff touches the windpipe lining) to ensure a good gas seal while avoiding windpipe injury.iTraXS measurements could also aid ETT placement and vital sign monitoring (oxygen saturation, heart rate, pulse volume, temperature) in pre-hospital conditions. This could replace multiple devices such as finger-clip oxygen monitors, which can be inconvenient on the battlefield or in an ambulance, or be inaccurate due to limb loss or low blood pressure, for instance.
Thanks to the new MRC funding, the researchers aim to develop regulatory-compliant software and hardware and expand the number and functionality of sensors built into iTraXS. At the end of the current project, the device will be ready for clinical trials and could be CE-marked and brought to market within three years.
Steve Morgan, Professor of Biomedical Engineering and Co-Director at the Centre for Healthcare Technologies, thinks the scope of iTraXS could be broadened to meet other healthcare needs with a range of different smart tubes. “Optical fiber sensing is a versatile platform technology that can measure a range of physical and biochemical parameters and could equally be applied to any internal catheter. With appropriate modification, such as a functional coating, the sensing capability can be significantly extended to monitor, for example, biofilm formation (bacterial growth) which is a major cause of infection,” he explains.
ITraXS has been developed in partnership with P3 Medical (Bristol, England), an ETT manufacturer, and Nottingham University Hospitals NHS Trust (NUH).
For more information, contact Steve Morgan at [email protected] or Emma Lowry, Media Relations Manager, at [email protected].
Source: University of Nottingham press release – November 23, 2020